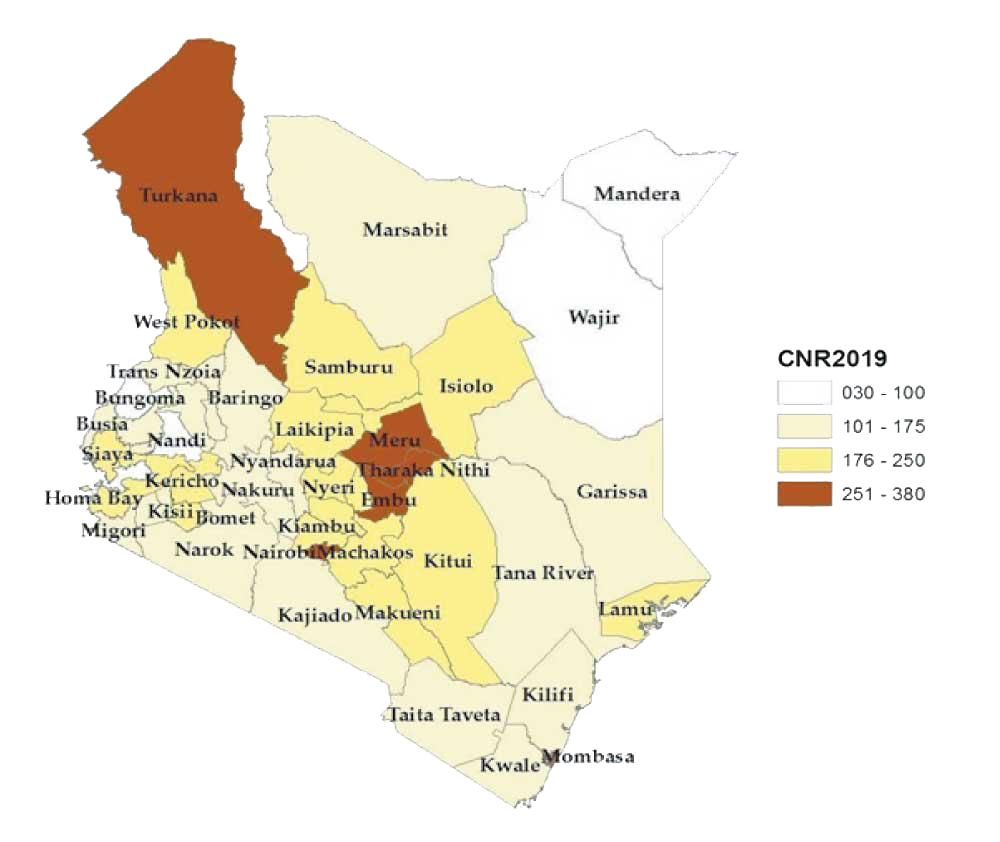
Kenya reported an increase in TB case notification between 2016 and 2018. However, the country reported a 10.4% decline in drug-susceptible TB (DS TB) cases, from 96,478 cases notified in 2018 to 86,385 cases in 2019. This can be attributed to operational challenges resulting in sub-optimal implementation of active case finding (ACF) in health facilities, delayed implementation of public-private mix (PPM) initiatives and widespread industrial action by healthcare workers in some counties.
Tuberculosis
Kenya continues to step up the fight against major communicable diseases that are of public health concern including Tuberculosis and HIV. In 2019, Kenya launched the first-ever patient-centred and costed National Strategic Plan (NSP) for Tuberculosis (TB), Leprosy and Lung health 2019-2023 with a vision of a Nation free from TB and Leprosy and reduced burden of Lung Diseases.
Age distribution
Age groups 20 – 44 and 60+ reporting more cases.
- Male
- Female
In 2019, 65% of DS TB cases notified were men, who were mostly within the 20-44 year age-groups and the elderly population above 60 years of age.
Paediatric Tuberculosis
Childhood TB continues to be a recognized global public health problem. Children are infected either directly from an index adult case or from reactivation of latent TB. The predisposing factors include: under-developed immunity, congested living conditions, malnutrition, congenital heart diseases, chronic deprivation and HIV disease among others.
TB HIV Comorbidity
HIV testing among TB patients remained high at 98% in 2019, with some counties like Nyamira and Homabay testing all patients with TB. Isiolo tested the least at 82%. HIV testing was similar across the genders but higher among adults at 98% as compared to children at 96%.
There was a slight decline in co-infection rate at 26% in 2019 as compared to 27% in 2018. The ART uptake was 96% with Uasin Gishu county reporting the least at 79%.
Latent Tuberculosis Infection (LTBI)
In line with WHO recommendations on the use of shorter rifapentine-based regimen (3-HP) for treatment of LTBI, the country embarked on an exercise of developing an LTBI policy document through the support of WHO. Two workshops were held in October and December 2019 to develop LTBI policy and a health care workers’ guideline on management of Latent TB infection. These workshops brought together technical officers from the National TB program, CTLCs representatives, NASCOP, KEMRI, members of the Civil society, patients’ advocates and representatives and partners including CHS, EGPAF, CDC, Stop-TB Partnership, NEPHAK, CHAI and WHO.
In 2019, the MOH procured Interferon Gamma Release Assay (IGRA) test kits for use in the testing for latent TB infection. Successful development of the health care workers’ sensitization package and subsequent training was conducted with support from CHAI.
- Numbers
Treatment Outcomes for Isoniazid Preventive Therapy
Among the under five children initiated on IPT, 81% completed treatment. This was an improvement of 30% compared to 2017 where 51% had an outcome of treatment completed. This is attributed to consistent sensitizations among health care workers on the need to track patients initiated on IPT.
- Treatment completed - 81%
- Died - 0.1%
- Discontinued - 1.1%
- Lost to follow up - 1.9%
- Not Evaluated - 16%
Isoniazid preventive therapy outcomes (2018 cohort) for under 5yrs
Nutrition
In 2017, the NTLD-P conducted a TB Patient Cost survey that indicated that between 27.1% and 53.7% of TB affected households experienced food insecurity. Additionally, the high cost drivers among the DR-TB patients were largely attributed to nutritional supplement while among DS-TB patients, the main cost drivers in order of cost were hours lost, nutritional supplements and direct medical costs.
In 2019, 45% of the diagnosed drug susceptible and 54% of drug resistant TB were undernourished at the time of diagnosis.
Unsteady supply chain management leading to untimely procurement of nutritional supplements affected provision of nutritional support to TB patients in 2019.
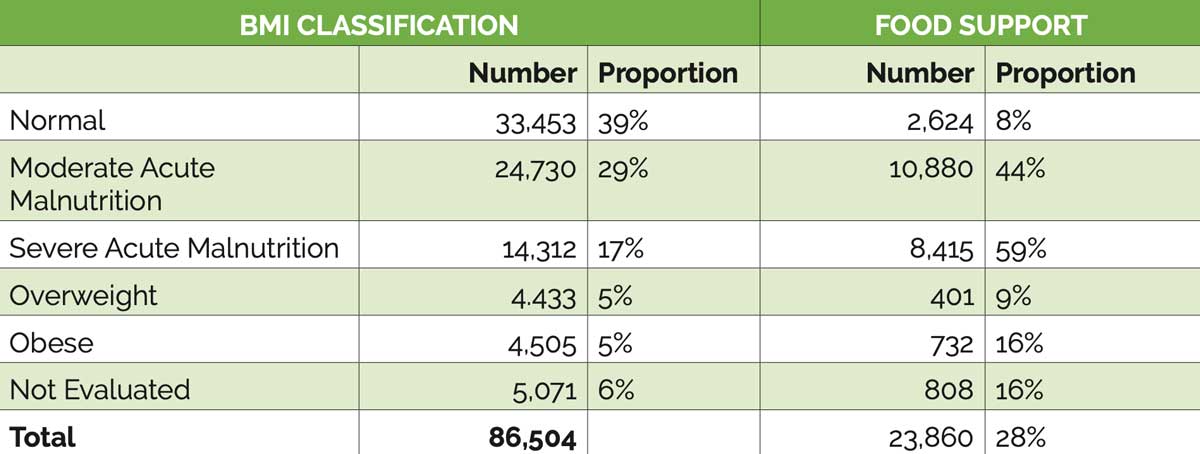
Nutritional Status of DSTB Patients in 2019
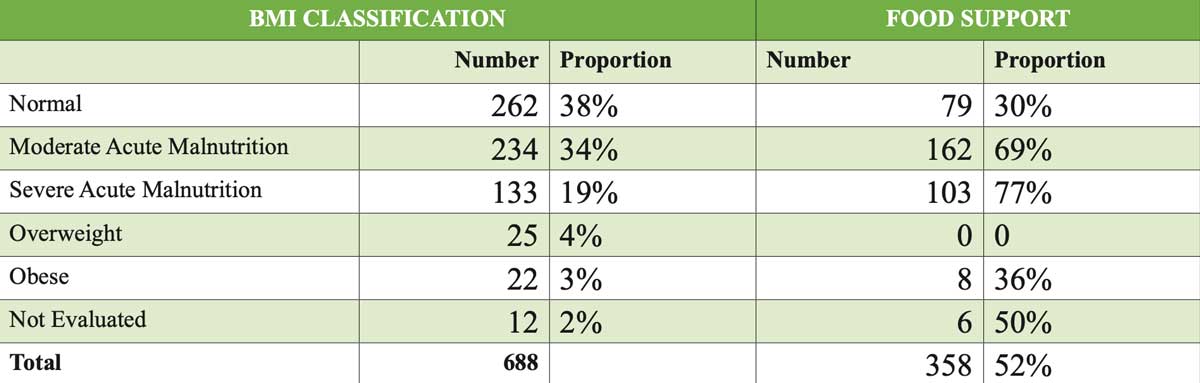
Nutritional Situation of DRTB Patients in 2019
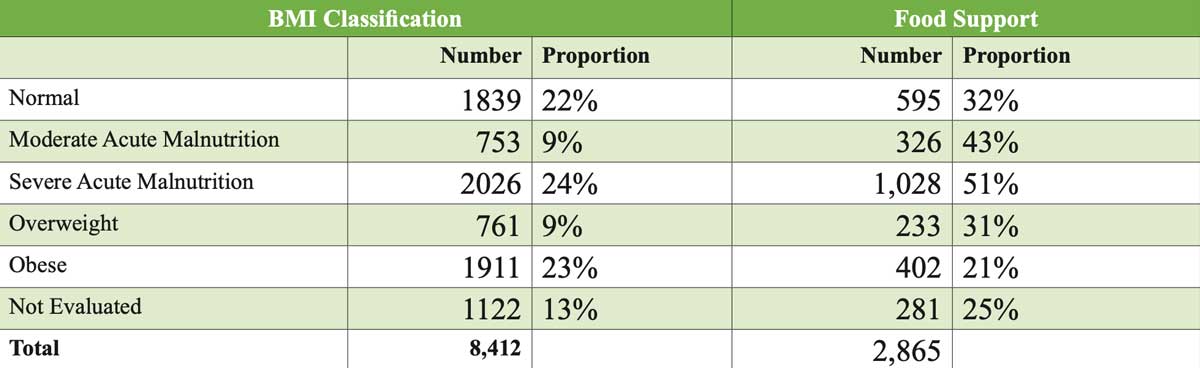
Nutritional Situation of Children, 2019
Current Risk
Why did we make Tuberculosis a focus area as an organization?
Notification rates of cases of tuberculosis (TB) in Kenya have increased six-fold in the past 15 years, largely as a result of the impact of the human immunodeficiency virus (HIV) on the disease, presenting substantial challenges to control of the disease. During this time, the coverage and quality of the national TB control programme (NTP) greatly improved, also contributing to the increased case notification rates.

What We've Done
Rhoncus modnam iaculis vitaenu dapibus lobortis uisque purusd nonmorbi. Euismo onec nislnam magnapro nuncproi potenti egestas massan. Erdum sed enimdon eget lectusa nec orciduis bulum ullamco malesu. Enas turpis eleifend sse msed uisque aesent.
Our Impact
Diampr egesta suscipit accumsan auctorpr lus. Snam ligulam quispr vamus ante dolornu iquam sollic odio. Lacusaen leocur vulput magnaa sduis velit euismo esent malesuad onec. Quispr roin himena iain temporse disse sellus oin que quamphas. Tortor oin mattiss massased potent ut quamve quat. Sit onec quisut ris viverr nisi isised. Nulla potenti lobortis consec adipisci litora lus disse.

The right to health is one of a set of internationally agreed human rights standards and is inseparable or ‘indivisible’ from all other rights.
Stories
CHS continues to grow as the preferred partner for health solutions by consistently focusing on the delivery of quality services and continuous improvement across all our program activities.
CHS continues to grow as the preferred partner for health solutions by consistently focusing on the delivery of quality services and continuous improvement across all our program activities.
TB Symptoms
The symptoms could be a combination or all of the following. Please seek medical attention should you experience these symptoms. Note that the symptoms are only used as a guide and test need to be done by a medical prationeer to ascertain whether or not a patient is suffering from TB.
TB FAQs
I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
TB treatment is fully subsidized by the MoH and is therefore free of charge for all persons seeking treatment in public health facilities countrywide.
In Kenya, the very young (<5years) and the elderly (>65years) are most at risk. However, the most affected age group is the reproductive age group (15 – 44years) where men are more affected than women. Additionally, key populations have been identified who include miners, people who inject drugs and those in congregate settings.
The commonest initial symptoms of TB include fever and cough. These are usually low grade and most times are perceived as not serious. This is the reason that most TB cases are diagnosed after a prolonged period of illness.
- Cough
- Fever
- Weight loss
- Drenching night sweats
- Chest pains
- Haemoptysis (Coughing blood stained sputum)
Additional symptoms/ signs in children.
- Failure to thrive
- Lethargy
No. Tuberculosis is a bacterial infection. Most people who are infected with tuberculosis do not exhibit any symptoms and can remain in a state of latent infection with TB. For those who progress to develop symptoms, the TB disease can resolve without any treatment in ~30%. Once treated though, Tuberculosis is completely curable and treatment clears all bacteria from the system.
Yes. One can contract TB even after vaccination. The vaccine for tuberculosis (BCG) protects children against severe forms of the disease (CNS and TB pericarditis)
Yes. TB is an airborne infection spread by droplets from an infected person to a susceptible host through speech, coughing, singing and sneezing. Due to this mechanism of spread, it is possible to be infected again after successful treatment. This is the reason why all contacts of confirmed TB cases are routinely screened and tested for TB to prevent re-infecting those who are treated.
Yes. TB can be cured as many times as one is infected. However, for those who have been previously treated, it is mandatory to exclude resistance to any of the anti-TB medicines.
Yes. In most instances, tuberculosis does not affect fertility. TB treatment does not affect fertility and it is important to inform your health worker if you are on hormonal contraception. The TB medicines could affect the function of these contraceptives leading to unplanned pregnancy.
Any child with TB can be treated at any public health facility for free. Kenya has introduced baby-friendly formulations of first line anti-TB medicines. This has ensured that it is possible and easy to treat all children with TB. Children tolerate medicines much better than adults.
TB Myths Vs Facts
| MYTHS | FACTS |
| If I have TB, do I also have HIV | NO. HIV increases one’s chance of getting TB. However, one can have TB without HIV |
| Can TB be inherited? | NO, it is not inherited. TB can only be spread through to close members of the same family living together, when the person coughs, laughs, sneezes, sings or spits. TB may occur in close family members because of close proximity but not because of inheritance. |
| Is TB a result of witchcraft? | NO, it is not. It is caused by a germ (bacteria) |
| Is TB a curse? | NO, it is not. It is a disease caused by a bacteria and is treatable and curable |